MACRA & MIPS COMPLIANCE
SPIN Compliance Solutions is the premier hands-on HIPAA, MACRA/MIPS, OSHA, Stark Law, and Anti-Kickback Statute Compliance Training Company serving medical practices in the continental US. We have been passionately saving physicians from compliance penalties since 2018. Our mission is simple... Take the time and frustration out of keeping your practice compliant so you can focus on your patients and practice.
If you want to take the frustration out of keeping your practice compliant then you won’t find an easier solution. Our hands-on compliance training and security audits provided by our exceptionally trained staff make it possible for you to focus on your practice. Contact us now so we can take the headache out of keeping you compliant today.
WHAT IS MACRA/MIPS COMPLIANCE?
For the last few years, clinicians have been required to comply with MACRA (the Medicare Access and CHIP Reauthorization Act of 2015), which enacts the Quality Payment Program. Many clinicians ask, “How do I comply with MACRA/MIPS so that I can avoid losing Medicare Part B money, but also not leave money on the table when I do comply?” The MACRA/MIPS legislation changes every year, which makes it very difficult for clinicians and practices to fully understand how to comply. SPIN helps client’s breakdown these changes so that they can not only fully comply with MACRA/MIPS, but also be able to get the highest possible increase to their Medicare Part B that they can get.
WHAT IS MACRA?
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) established the Medicare Quality Payment Program (QPP) to reward high-value, low-cost care. Eligible clinicians annually choose to participate in one of two payment tracks, the first is called the Merit-Based Incentive Payment System (MIPS).
WHAT IS MIPS?
The Merit-Based Incentive Payment System (MIPS). Under MIPS, eligible clinicians continue to be paid on a fee-for-service basis and report cost and quality data. Following each performance year, clinicians are evaluated on their performance relative to other clinicians in the country and receive a positive, neutral, or negative payment adjustment to their Medicare Part B payments two years later. For example, 2021 performance will impact 2023 payments.
HOW MIPS WORKS
Each clinician that is eligible to report MIPS data will submit quality, promoting interoperability, and improvement activities data they collect during the performance year. CMS collects and calculates cost measures for the clinician or group. The 4 performance categories are scored and make up each clinician’s or group’s MIPS final score. The final score determines the Medicare Part B payment adjustment. The 4 categories are:
Quality
There are over 200 quality measures to pick from. Each clinician, or group, must collect and report data on at least 6 quality measures. QPP has set up specialty-specific measures, but clinicians may pick any of the 200 plus measures to collect and report data on. A clinician or group must report performance data for at least 70% of the patients who qualify for each measure. Data can be submitted through your EMR system, through claims, or through registries. The Quality category currently makes up 30% of the clinician’s or group’s overall MIPS score.
Promoting Interoperability
The Promoting Interoperability category requires you to use an Electronic Health Record/Electronic Medical Record (EHR/EMR) system that meets the 2015 Edition certification criteria, 2015 Edition Cures Update certification criteria, or a combination of both for participation in this performance category. A clinician or group must submit collected data for specific measures from each of the 4 objectives measures (unless an exclusion is claimed) for the same 90 continuous days (or more) during the performance year. In addition to submitting measures, you must provide your EHR/EMR’s CMS Identification code from the Certified Health IT Product List (CHPL) and attest to several specific questions. Hardship exceptions do apply to the Promoting Interoperability category, and if the clinician or group is granted the exception then the 25% score for this category is transferred to the Quality Category Score.
Providing The Best Hands-On MIPS And MACRA Compliance Training Programs To Medical Practices in St. Louis, MO., Atlanta, GA., Houston, TX., Philadelphia, PA., Hershey, PA., Oklahoma City, OK., Reno, NV., Orlando, FL., Detroit, MI., Orange County, CA and the continental United States.
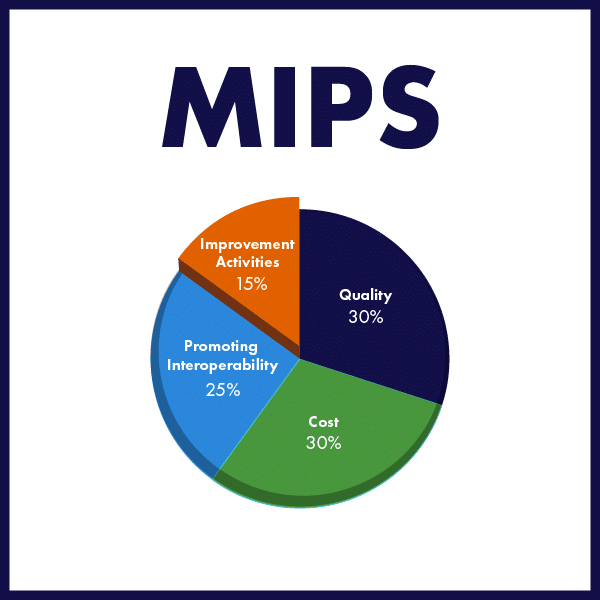
Improvement Activities
Clinicians and groups in this category earn full credit by submitting one of the following combinations of activities:
- 2 high-weighted activities,
- 1 high-weighted and 2 medium-weighted activities, or 4 medium-weighted activities
- This category requires performance by the clinician and/or group for a continuous 90 day performance.
- If you are considered a small group, or are identified as a clinician that works for a small group, then you are required to submit one of the following combinations of activities:
- 1 high-weighted activities
- 2 medium-weighted activities
- Small groups are groups that have less than 15 clinicians.
- This category makes up 15% of the overall MIPS Score
Cost
The clinician and group that is reporting MIPS data, does not report anything for the Cost category. CMS uses Medicare Part A and B claims data to calculate cost measure performance for each clinician or group. There are several cost measures that CMS will look at and determine if the group or clinician meet that measure. This category makes up 30% of the overall MIPS score.
We specialize in HIPAA, MIPS, OSHA, Medicare/Medicaid Audits, and more. View our services and see how we can help your medical practice today.
Our program offers cost-effective solutions to organizations so you can avoid HIPAA audits and monetary fines. Call Us Today!
WHY IS IT IMPORTANT TO NOT JUST RELY ON YOUR EMR/EHR SYSTEM TO REPORT YOUR MIPS DATA?

To determine if a clinician or group is required to report MIPS data each year, they must meet or exceed the Low-Volume Threshold. The low volume threshold includes 3 aspects of covered professional services; (1) allowed charges; (2) Number of Medicare patients who receive services; (3) Number of services provided. A clinician or group must participate in MIPS, there for is eligible to report MIPS data, if, in a 12-month period (Jan – Dec each year), they:
- Bill more than $90,000 for Part B covered professional services, and
- See more than 200 Part Be Patients, and;
- Provide more than 200 covered professional services to Part B patients
If the clinician or group are brand new to Medicare, then they are exempt from reporting MIPS data for that performance year. However, it is best to begin complying with all of MIPS requirements now so that when the clinician or group have to report, they are ready to do so without any penalty.
WHO HAS TO REPORT MACRA/MIPS DATA EACH YEAR?
To determine if a clinician or group is required to report MIPS data each year, they must meet or exceed the Low-Volume Threshold. The low volume threshold includes 3 aspects of covered professional services; (1) allowed charges; (2) Number of Medicare patients who receive services; (3) Number of services provided. A clinician or group must participate in MIPS, there for is eligible to report MIPS data, if, in a 12-month period (Jan – Dec each year), they:
• Bill more than $90,000 for Part B covered professional services, and
• See more than 200 Part Be Patients, and;
• Provide more than 200 covered professional services to Part B patients
If the clinician or group are brand new to Medicare, then they are exempt from reporting MIPS data for that performance year. However, it is best to begin complying with all of MIPS requirements now so that when the clinician or group have to report, they are ready to do so without any penalty.
WHAT IS THE BEST WAY TO ENSURE I MEET ALL THE REQUIREMENTS AND MY MIPS SCORE IS THE BEST IT CAN BE?
Each clinician and group should get someone to help them that knows these laws and can advise on them. Most MIPS compliance companies do not have anyone that can advise on these laws, as they do not employ attorneys. Also, clinicians and groups must make sure that they have a dedicated MIPS team, which should be made up of IT personnel, clinicians, support staff, and legal staff, so that the team can monitor and periodically report on how the group and/or clinician is doing with their MIPS performance. Failure to take this seriously can cause a clinician and/or group to lose up to 9% of their Medicare Part B reimbursement.